Introduction to Kidney Function Regulation
The kidneys' function is efficiently monitored and regulated by a hormonal feedback control mechanism involving the hypothalamus, juxtaglomerular apparatus, and, to some extent, the heart. Changes in blood volume, body fluid volume, and ionic concentration activate hypothalamic osmoreceptors. When there is an excessive loss of fluid from the body or an increase in blood pressure, the hypothalamic osmoreceptors respond by stimulating the neurohypophysis to secrete an antidiuretic hormone (ADH) or vasopressin (positive feedback).
The average kidney is about the size of a cell phone and weighs about 4-6 ounces. Despite accounting for only 0.5% of the body's weight on average, the kidney receives more blood than all other organs except the liver. Nephrons are the kidney's filtering units, and each kidney has between 1 and 2 million nephrons.
In this article, we will look into the different roles of these hormones which regulate the functioning of kidneys and also look into the structure and the function of this amazing organ.
Regulation of Kidney Function
Urine is described as a liquid or semi-solid solution of generated waste by physiological functions which also contains hazardous chemicals created by excretory organs during fluid circulation. Waste is often expelled from the human body in the form of urine. In the excretion process, our kidneys play an important role. It is made in the nephron, which is the kidney's structural and functional unit.
The kidney's major purpose is to produce urine and purify the blood. The kidney filters waste and other compounds that are no longer needed by the body. All the activities and functions in the kidney are regulated by the body by releasing some hormones and autoregulation. In autoregulation, the kidney regulates its function with the help of its structures and cells.
Different stages such as filtration, reabsorption, and secretion during urine formation are regulated. The pituitary gland is stimulated by changes in urine flow and bodily fluids to release hormones that control the pituitary gland's activity, including vasopressin (ADH), renin, and aldosterone.
Kidney Structure
The kidney is a part of the excretory system and helps in urine formation and excretion from the body. Some facts are given below about the kidney:
The kidneys are two bean-shaped organs.
It is divided into two areas: a dark outer area (the cortex) and a lighter inner area (the medulla).
There are 10 to 18 renal pyramids in the medulla, which are triangular structures with a striped appearance. The renal tubules and related blood arteries give them this appearance.
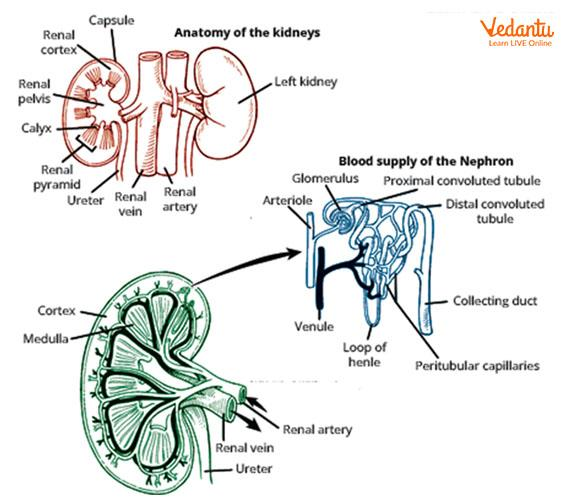
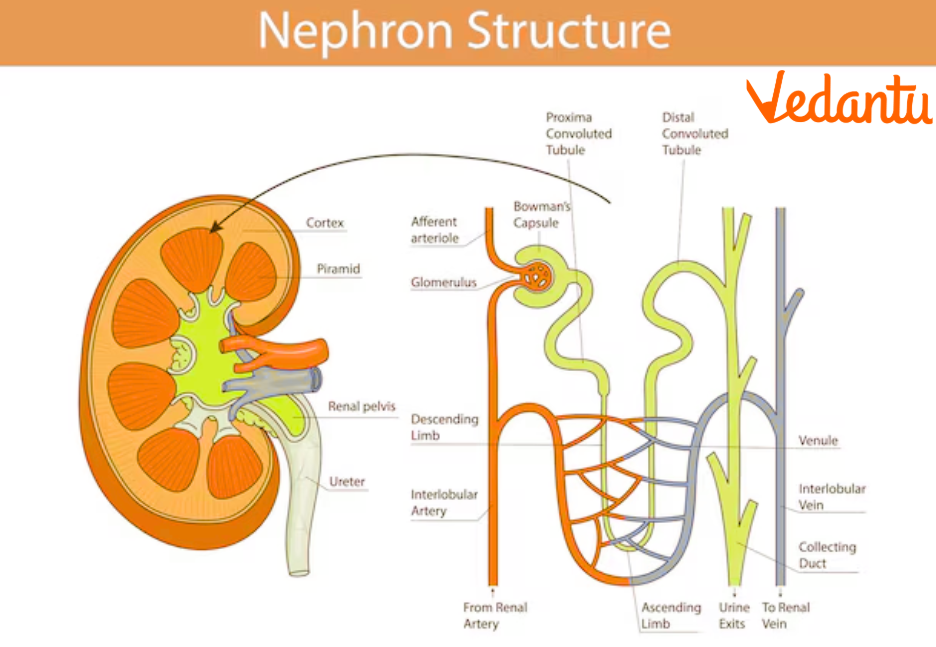
Structure of Kidney and Nephron
Waste is often expelled from the human body in the form of urine.
Urine is made in the nephron, which is the basic structural unit of a kidney.
Nephrons are important as they are the functional and structural units in the kidney. The nephrons, which filter the whole volume of blood in the body 60 times a day, are the backbone of the urinary system.
Nephron has a glomerulus, Bowman’s capsule, and renal tubules. Bowman's capsule is the first segment of the renal tube, which surrounds the glomerulus and receives the filtrate from the glomerular capillaries. The glomerulus is a capillary network in the kidney that performs as a filtration site.
Function of Kidney and Its Structure
The structures of the kidney have different functions in urine formation and regulation.
Renal Capsule: It covers the outer surface of the kidney and helps in the ultrafiltration of the urine.
Renal Medulla: It is the innermost part of the kidney that consists of nephrons and helps in urine formation.
Medullary Pyramid: It carries urine from the collecting ducts to the calyx.
Major and Minor Calyx: These carry the urine to the renal pelvis of the kidney.
Renal Pelvis: It collects urine from the kidney and passes it to the ureter.
The primary function of the kidneys is to maintain equilibrium. They make the body's internal environment stable and comfortable by controlling fluid levels and balancing electrolytes and other elements.
It produces a variety of hormones and enzymes, including erythropoietin, which is a hormone that is produced in response to hypoxia, and Renin regulates angiotensin and aldosterone, which regulates blood pressure.
Hormones That Regulate the Kidney Function
Renin, angiotensin II, prostaglandins, bradykinin, ADH, aldosterone, ANP, vitamin D, PTH, and erythropoietin are the hormones involved in the hormonal regulation of the kidneys.
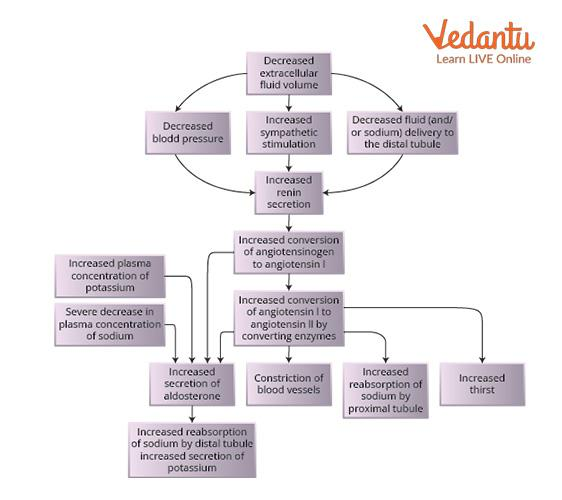
Juxtaglomerular (JG) Apparatus
The granular cells (juxtaglomerular cells) in the JGA's glomerular arterioles (especially the afferent) are specialised, smooth muscle cells in the wall (juxtaglomerular apparatus). These JG cells are responsible for the production of renin.
Renin levels are increased by the renal sympathetic nerves through a direct action on granular cells (mediated by beta1-adrenergic receptors) and a decrease in flow to the macula densa.
Increased renal sympathetic nerve activity causes a drop in GFR and an increase in proximal sodium ions and water reabsorption, both of which reduce the amount of fluid supply to the macula densa. This further helps in renin production at a high level.
The Renin-Angiotensin-Aldosterone System
The precursor angiotensinogen is synthesised in the liver.
The stimulation of the kidney increases the production of renin, an enzyme that converts angiotensinogen to angiotensin I by a cleavage mechanism that reduces the polypeptide from 453 to 10 amino acids.
Angiotensin is an enzyme in the endothelium that converts angiotensin I to angiotensin II.
Angiotensin II stimulates vasoconstriction in the cardiovascular system, stimulates aldosterone production in the adrenal glands, and increases sodium reabsorption in the kidneys, which enhances both salt and water reabsorption.
The vasoconstrictor actions along with salt and water retention result in an overall effect of blood pressure elevation. Angiotensin II functions as a vasoconstrictor in the arterial wall and induces Aldosterone synthesis in the adrenal glands. It also promotes salt reabsorption within the kidneys. It acts on the adrenal cortex to enhance aldosterone secretion, as well as the kidneys themselves, due to increased salt and water accumulation.
Hypothalamus
Antidiuretic Hormone(ADH)
The hypothalamus produces ADH in neurosecretory cells, which then carry it down their axons to nerve terminals in the posterior pituitary gland, where it is stored.
Blood plasma levels are monitored by osmoreceptor cells in the hypothalamus.
If the concentration is too high, signals are sent to ADH neurosecretory cells, causing ADH to be produced from the posterior pituitary nerve terminals.
ADH produces a decrease in blood plasma concentration by increasing water uptake in the kidney collecting duct.
When osmoreceptors detect a decline in blood plasma levels, the neurosecretory cells are not triggered to release ADH, and the blood ADH level drops, resulting in dilute urine.
Atrial Natriuretic Peptide (ANP)
It is a 28-amino-acid peptide hormone found in granules in atrial myocytes, particularly in the right atrium.
Increased blood flow in the atria of the heart causes ANP to be released. The renal tubules, particularly in the collecting duct, are then inhibited from reabsorbing salt and water. Reduced sodium ion and water levels enhance urine output, allowing blood volume to return to normal.
It reduces aldosterone secretion from the adrenal cortex as well as renin release, lowering angiotensin levels.
Regulation of Kidney Function Flow Chart
Kidney Failure- Causes, Symptoms, and Treatment
Kidney failure refers to the inability of the kidneys to effectively filter blood and perform essential functions such as toxin removal, fluid balance, and waste elimination. When kidney function becomes insufficient, it can lead to serious health problems due to the accumulation of waste products and toxins in the bloodstream.
Types of Kidney Failure
Acute Kidney Failure – Sudden loss of kidney function, often due to infection or injury.
Chronic Kidney Failure – Gradual decline in kidney function over time, often due to conditions like diabetes or high blood pressure.
When the kidneys stop working, toxins and waste build up in the blood, causing life-threatening complications.
Causes of Kidney Failure
Some common causes of kidney failure include-
Kidney dysfunction or disease
Uncontrolled high blood pressure (hypertension)
Diabetes
Prolonged use of anti-inflammatory drugs
Chronic health conditions
Severe dehydration
Drug abuse
Infections or disorders of the excretory system
Kidney Diseases Leading to Kidney Failure
Several kidney diseases and disorders contribute to kidney failure, including-
Renal Calculi (Kidney Stones)
Glomerulonephritis (inflammation of the kidney’s glomeruli)
Urethritis
Pyelonephritis
Cystitis
Hematuria (blood in urine)
The kidneys are vital for filtering waste, balancing fluids, and regulating blood pressure. They rely on hormones like ADH and aldosterone to function properly. When kidneys fail, due to causes like diabetes or high blood pressure, it can lead to serious health problems. Taking care of your kidneys with a healthy lifestyle is key to avoiding kidney failure and maintaining overall health.
Essential Study Materials for NEET UG Success
FAQs on Regulation of Kidney Function: Key Hormones and Mechanisms for NEET
1. What is the main function of the kidneys?
The main function of the kidneys is to filter waste products and excess fluid from the blood, producing urine. They also help regulate blood pressure and maintain electrolyte balance.
2. How do the kidneys regulate body fluids?
The kidneys regulate body fluids through filtration, reabsorption, and secretion processes in the nephron, using hormones like ADH, aldosterone, and renin to control water and salt balance.
3. What hormones are involved in kidney function regulation?
The key hormones involved are ADH (antidiuretic hormone), aldosterone, renin, angiotensin II, ANP (atrial natriuretic peptide), and erythropoietin.
4. What is the role of ADH in kidney function?
ADH helps regulate water balance by increasing water reabsorption in the kidneys, reducing urine output when the body is dehydrated or when blood plasma levels are high.
5. How does the renin-angiotensin-aldosterone system (RAAS) affect kidney function?
RAAS regulates blood pressure by stimulating vasoconstriction, increasing sodium reabsorption in the kidneys, and triggering the release of aldosterone, which helps balance fluid levels and blood pressure.
6. What is the function of the juxtaglomerular apparatus (JGA)?
The JGA detects changes in blood pressure and sodium levels, and it produces renin to regulate blood pressure and fluid balance in the kidneys.
7. What causes kidney failure?
Kidney failure can be caused by factors such as uncontrolled high blood pressure, diabetes, infections, kidney diseases like glomerulonephritis, and prolonged use of certain medications.
8. What is glomerulonephritis?
Glomerulonephritis is the inflammation of the glomeruli in the kidneys, often caused by infections or autoimmune conditions, which can lead to kidney damage and failure.
9. What are the symptoms of kidney failure?
Symptoms include fatigue, swelling, high blood pressure, decreased urine output, blood or protein in urine and severe cases, nausea and confusion.
10. How is kidney function regulated by the hypothalamus?
The hypothalamus monitors blood plasma concentration and releases ADH from the posterior pituitary gland to adjust water levels in the body, aiding in fluid balance.