Functions and Clinical Importance of the Hepatic Portal System
The hepatic portal system is a specialized network of veins playing a vital role in human physiology. Unlike most veins, which carry blood directly toward the heart, this system collects blood from the digestive organs and channels it to the liver first. This process ensures that nutrients and other absorbed substances, including potential toxins, are processed by the liver before entering the wider circulatory system.
Anatomy and Structure of the Hepatic Portal System
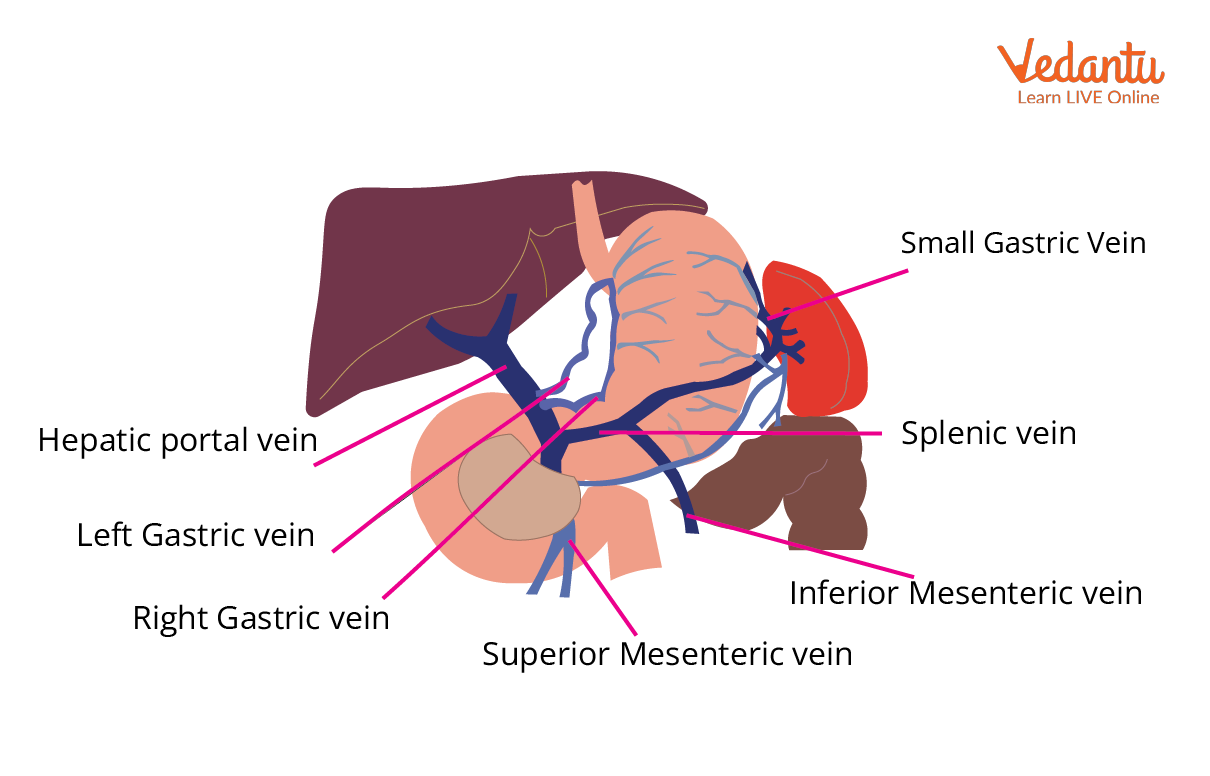
The hepatic portal vein is central to the hepatic portal system. It measures about 8 centimeters in adults and is located in the upper right quadrant of the abdomen, beginning behind the neck of the pancreas. Usually, it is formed by the joining of the superior mesenteric vein and the splenic vein—a point known as the splenic-mesenteric confluence.
In some cases, the inferior mesenteric vein also joins directly. Additional minor veins like the cystic and gastric veins may contribute to this system through various anatomical connections.
The hepatic portal vein delivers approximately 70% of the liver’s blood supply, with the remaining 30% coming from the hepatic artery. Blood enters the liver through the porta hepatis, a key gateway that also allows the hepatic artery in and lets bile exit. Within the liver, the portal vein splits into right and left branches, which further divide into smaller portal venules running alongside tiny hepatic arterioles.
How Blood Flows Through the Hepatic Portal System
The unique pathway of the hepatic portal system involves two successive capillary beds.
- Blood from the stomach, intestines, pancreas, and spleen is collected by various veins.
- These veins (superior mesenteric, inferior mesenteric, splenic, and gastric veins) converge to form the hepatic portal vein.
- The hepatic portal vein enters the liver and branches extensively.
- Portal venules and hepatic arterioles run together, creating a network called the hepatic portal triad, which is completed by the bile duct.
- Blood enters liver sinusoids, where mixing of venous and arterial blood occurs.
- Processed blood from each liver lobule collects in central veins, which merge into right and left hepatic veins.
- These hepatic veins exit the liver and empty into the inferior vena cava, returning blood to general circulation.
Functional Significance of the Hepatic Portal System
The hepatic portal system ensures nutrient-rich blood from food is efficiently processed before reaching the rest of the body. Immediately after eating, blood leaving the intestines is rich in nutrients and other absorbed substances. The portal system delivers this blood to the liver, which then:
- Metabolizes carbohydrates, proteins, and fats; stores glucose as glycogen
- Synthesizes vital proteins and other compounds
- Detoxifies drugs and other harmful substances
- Removes bacteria and debris picked up from the intestines
Hepatocytes, the main liver cells, perform these processes, preparing safe and useful nutrients for the body.
Key Definitions and Components
| Term | Summary |
|---|---|
| Hepatic Portal Vein | The main vessel bringing blood from digestive organs to the liver |
| Porta Hepatis | The gateway of the liver where the portal vein and hepatic artery enter and bile exits |
| Hepatic Sinusoids | Liver capillaries where mixing of portal and arterial blood occurs |
| Hepatocytes | Liver cells carrying out metabolism and detoxification |
| Hepatic Vein | Carries processed blood away from the liver to the inferior vena cava |
Clinical Relevance: Portal Hypertension
When pressure within the portal vein rises—known as portal hypertension—it signals serious liver disorders. Often, cirrhosis (scarring of liver tissues) is a typical underlying cause. Effects can include:
- Ascites (fluid build-up in the abdomen)
- Esophageal varices (swollen veins that may bleed)
- Skin changes (spider nevi, caput medusae, palmar erythema)
Prompt recognition and treatment of portal hypertension are essential in clinical settings.
Comparative Portal Systems
| Portal System | Origin | Destination | Main Function |
|---|---|---|---|
| Hepatic Portal System | Digestive organs | Liver | Metabolism, detoxification, nutrient processing |
| Hypophyseal Portal System | Hypothalamus | Pituitary gland | Hormonal regulation |
Example Questions and Practice
To solidify your understanding of the hepatic portal system:
- List the organs whose veins ultimately form the hepatic portal vein.
- Draw and label a basic schematic of the hepatic portal system, showing all key vessels.
- Describe the steps blood takes from the small intestine to the heart, specifically highlighting its path through the liver.
Explore more resources and diagrams on the Hepatic Portal System at Vedantu.
Conclusion
The hepatic portal system stands as a central checkpoint between digestion and circulation, safeguarding the body by letting the liver process, detoxify, and store nutrients before blood travels further. Understanding its pathway and function is key for mastering core concepts in biology and human health.
FAQs on Hepatic Portal System Explained: Structure, Pathway & Role
1. What does the hepatic portal system do?
The hepatic portal system is responsible for transporting blood from the digestive organs to the liver. This enables the liver to process nutrients, detoxify harmful substances, and metabolize chemicals before blood enters the systemic circulation. It is a crucial component of human physiology.
2. Which organs drain into the hepatic portal system?
The hepatic portal system receives blood from several digestive organs, including:
- Stomach
- Small intestine
- Large intestine
- Pancreas
- Spleen
These organs send nutrient-rich venous blood through the portal vein to the liver for further processing.
3. Define hepatic portal vein.
The hepatic portal vein is the major vein that carries blood from the gastrointestinal tract and spleen to the liver. It is formed by the union of the superior mesenteric vein and splenic vein. This vein delivers nutrient-rich, but oxygen-poor, blood to the liver for filtration and metabolism.
4. What are the three types of portal systems in humans?
The three types of portal systems found in humans are:
- Hepatic portal system (connects GI tract to liver)
- Hypophyseal portal system (connects hypothalamus to anterior pituitary)
- Renal portal system (found in lower vertebrates, not functional in adult humans)
5. What is the function of the hepatic portal system?
The main function of the hepatic portal system is to deliver nutrient-rich blood from the digestive organs to the liver. The liver then processes nutrients, detoxifies toxins, stores glucose as glycogen, and breaks down harmful substances before allowing the blood to enter systemic circulation.
6. What is the difference between the hepatic vein and the hepatic portal vein?
The hepatic portal vein carries blood from the digestive organs to the liver, while the hepatic vein transports filtered blood from the liver to the inferior vena cava. In summary:
- Hepatic portal vein: From GI tract/spleen to liver
- Hepatic vein: From liver to heart (via inferior vena cava)
7. Why is the hepatic portal system important in metabolism?
The hepatic portal system is essential because it allows the liver to regulate, store, and metabolize nutrients immediately after absorption. This 'first-pass effect' ensures harmful substances are detoxified and nutrients such as glucose, amino acids, and fats are efficiently processed before reaching the rest of the body.
8. What veins form the hepatic portal vein?
The hepatic portal vein is primarily formed by the union of the superior mesenteric vein and the splenic vein. The inferior mesenteric vein usually drains into the splenic vein, and additional contributory veins include the left and right gastric veins, and the pancreaticoduodenal veins.
9. What happens to the blood once it enters the liver through the hepatic portal system?
Once blood enters the liver via the hepatic portal vein, it passes through liver sinusoids, where:
- Nutrients are absorbed, stored, or converted
- Toxins are detoxified
- Pathogens are filtered
The processed blood then leaves the liver through hepatic veins into the inferior vena cava.
10. How does the hepatic portal system differ from systemic circulation?
The hepatic portal system channels blood through two capillary beds in sequence (digestive organ and liver), whereas systemic circulation delivers blood directly from arteries to organs and returns it via veins to the heart. This ensures that the liver processes absorbed substances before they enter the general circulation.
11. What is portal hypertension and how does it relate to the hepatic portal system?
Portal hypertension is increased blood pressure within the hepatic portal system, often caused by liver diseases like cirrhosis. It can result in:
- Ascites (fluid accumulation in the abdomen)
- Varices (swollen veins, especially in the esophagus)
- Caput medusae (dilated abdominal veins)
These complications arise due to obstructed blood flow through the liver.
12. Can you give a simple mnemonic to remember the main veins of the hepatic portal system?
Yes, an easy mnemonic is “SIS-GPS”:
- Splenic vein
- Inferior mesenteric vein
- Superior mesenteric vein
- Gastric veins
- Pancreatic veins
- Splenic vein (again, as the key convergence point)