How to Read Blood Group Test Results Accurately
A blood group test is a basic yet crucial investigation that identifies the specific category of blood an individual possesses. There are different blood group test names for this, but most commonly it is referred to as ABO typing (to check whether you are Group A, B, AB, or O) and Rh typing (positive or negative). Knowing your blood type helps doctors make safe decisions in emergencies, especially when a blood transfusion is required. In this guide, we will discuss the blood group test procedure, the essential materials needed, how to interpret the blood group test chart, and what to keep in mind when reviewing a blood group test report.
What is a Blood Group Test?
A blood group test determines which antigens are present on the surface of your red blood cells. These antigens are generally classified under the ABO Blood Group System and the Rh factor. Testing your blood type accurately is necessary for safe blood transfusions, organ transplants, and even in certain medical conditions where blood grouping is mandatory.
The ABO Blood Group System
The ABO Blood Group System was discovered by Karl Landsteiner. It is based on the presence or absence of two primary antigens—A and B.
Group A: Has antigen A on the red blood cells and antibody B in the plasma.
Group B: Has antigen B on the red blood cells and antibody A in the plasma.
Group AB: Has both antigens A and B on the red blood cells and no A or B antibodies in the plasma.
Group O: Has no A or B antigens on the red blood cells but has both A and B antibodies in the plasma.
The Rh Factor
Apart from the A and B antigens, the Rh factor (mainly the D antigen) further classifies blood types into Rh-positive (D antigen present) or Rh-negative (D antigen absent). Consequently, each of the four ABO blood groups can either be Rh-positive or Rh-negative, giving rise to eight possible blood types:
A+
A-
B+
B-
AB+
AB-
O+
O-
Materials Required for a Blood Group Test
A blood group test kit typically contains everything you need to perform the test at home or in a lab setting:
A clean glass slide
Monoclonal antibodies (Anti-A, Anti-B, and Anti-D)
Lancet (for finger prick)
Alcohol swabs
Sterile cotton balls
Toothpicks (or similar stirrers)
Biohazard disposal container
Blood Group Test Procedure
Below is the simple blood group test procedure commonly followed in many labs and also doable at home with the right precautions:
Mark the Slide: Draw three separate circles on a clean glass slide.
Add Reagents: Place a drop of Anti-A in the first circle, Anti-B in the second, and Anti-D in the third.
Prepare the Finger: Clean your ring finger with an alcohol swab and allow it to dry.
Prick and Discard: Prick your fingertip gently with the lancet. Wipe off the first drop of blood using a cotton ball.
Collect Blood Drops: Carefully allow one drop of blood to fall on each circle by gently pressing your finger.
Mix Thoroughly: Use separate toothpicks to mix the blood with the antibodies in each circle.
Observe for Clumping: Look for agglutination (clumping). If clumping occurs in Anti-A, you have antigen A; if it occurs in Anti-B, you have antigen B; if it occurs in Anti-D, you are Rh-positive.
Dispose Safely: Discard all materials (including the slide and toothpicks) into a biohazard container.
Blood Group Test Chart
The blood group test chart helps to interpret the outcomes. If your blood reacts (clumps) with:
By checking combinations:
Clumps in Anti-A only → Group A
Clumps in Anti-B only → Group B
Clumps in both Anti-A and Anti-B → Group AB
No clumps in Anti-A or Anti-B → Group O
Clumps in Anti-D → Rh+; No clumps in Anti-D → Rh-
Blood Group Test Report: Understanding the Results
A blood group test report typically mentions the ABO group and the Rh type. For instance, if you are A+ (A positive), your red cells have the A antigen and the Rh factor. This knowledge is important during emergencies or surgeries when you may need blood from a matching donor.
Universal Donor and Recipient:
Group O-: Universal donor, as it lacks A, B, and Rh antigens.
Group AB+: Universal recipient, as it contains both A and B antigens and the Rh factor, making it compatible with all other groups in emergencies.
Additional Tips for Accuracy
Use a Fresh Lancet: Always use a new sterile lancet to prevent infection and cross-contamination.
Clean the Finger Properly: Ensure the site is disinfected with an alcohol swab.
Dispose of Materials Safely: Contaminated items must go into a biohazard disposal container.
Check Expiry: If you are using a blood group test kit, make sure the reagents (Anti-A, Anti-B, Anti-D) are not expired.
Quiz Time
Test your understanding of the topic with the short quiz below:
1. Which blood group is known as the universal recipient?
a. B+
b. O-
c. AB+
d. A-
Answer: c. AB+
2. What does the Anti-D reagent test for?
a. Antigen D, which indicates the Rh factor
b. Antibody A in plasma
c. Antibody B in plasma
d. Presence of haemoglobin
Answer: a. Antigen D, which indicates the Rh factor
3. What is the rarest blood type globally?
a. O+
b. AB-
c. A+
d. B-
Answer: b. AB-
4. Which blood group can donate to all groups?
a. B+
b. AB-
c. O-
d. O+
Answer: c. O-
Related Topics


FAQs on Blood Group Test: Procedure, Chart, and Essential Tips for Students
1. What is the basic principle behind a blood group test?
The principle of a blood group test is based on an antigen-antibody reaction. Red blood cells (RBCs) have specific antigens on their surface. The test involves mixing a blood sample with laboratory-prepared antibodies (antisera for A, B, and D antigens). If the corresponding antigen is present on the RBCs, it will react with the antibody, causing the blood cells to clump together, a process called agglutination. This clumping pattern reveals the blood type.
2. What are the main steps involved in the slide method for blood typing?
The slide method, often used in school labs and for quick screening, involves a few key steps:
Sample Collection: A clean glass slide is divided into three sections, and a drop of blood is placed in each.
Reagent Addition: A drop of Anti-A serum is added to the first blood drop, Anti-B serum to the second, and Anti-D (for Rh factor) to the third.
Mixing: Each sample is mixed gently with a separate, clean applicator stick.
Observation: The slide is observed for agglutination (clumping). The presence or absence of clumping in each section determines the ABO blood group and Rh status.
3. Why is it so important to know a person's blood group?
Knowing a person's blood group is critical for several medical reasons, primarily for safe blood transfusions. Transfusing incompatible blood can cause a severe, life-threatening immune reaction. It is also essential during pregnancy to manage potential Rh incompatibility between the mother and fetus, and it plays a role in organ transplantation and certain genetic studies.
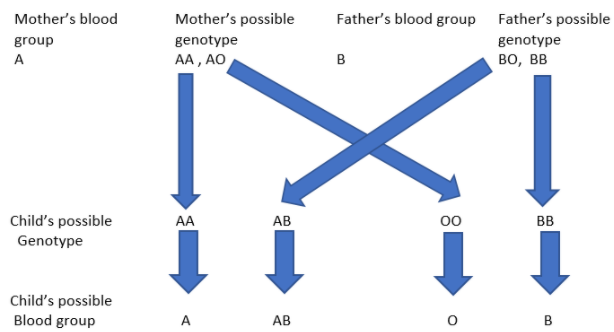
4. How are blood groups inherited from parents?
Blood groups are determined by genes inherited from our parents. For the ABO system, a child receives one allele (a version of a gene) from each parent. The A and B alleles are codominant, while the O allele is recessive. For example, if a child inherits an A allele from one parent and an O allele from the other, their blood type will be A. Similarly, the Rh factor (positive or negative) is also inherited independently.
5. What is the difference between the ABO system and the Rh system?
The main difference lies in the specific antigens involved:
The ABO system classifies blood based on the presence or absence of two antigens, A and B, on the surface of red blood cells. This results in four main types: A, B, AB, and O.
The Rh system classifies blood based on the presence or absence of the D antigen, commonly known as the Rh factor. If the D antigen is present, the blood type is Rh-positive (+); if it's absent, it's Rh-negative (–).
A complete blood type includes both system classifications, such as A+ or O-.
6. Why is blood group O- called the 'universal donor'?
Blood group O- is called the universal donor because its red blood cells lack A, B, and Rh (D) antigens. Since there are no antigens on the cell surface to trigger an immune response, O- red blood cells can be safely transfused to individuals of any ABO and Rh blood type, making it invaluable in emergencies when the recipient's blood type is unknown.
7. Can a person's blood group change over time?
Under normal circumstances, a person's genetically determined blood group remains the same throughout their life. However, in very rare medical situations, such as a bone marrow transplant from a donor with a different blood type, the recipient's body may start producing blood cells corresponding to the donor's blood type. This is an exception and not a natural change.
8. What determines if someone is a 'universal recipient'?
A person with AB+ blood is known as the universal recipient. This is because their red blood cells have both A and B antigens, and their plasma does not contain antibodies against A or B antigens. They are also Rh positive. Consequently, their immune system will not attack red blood cells from any ABO or Rh blood group, allowing them to receive blood from any donor.
9. Besides transfusions, what is another important application of blood typing?
Besides transfusions, blood typing is crucial in forensic science. Bloodstains found at a crime scene can be typed and used to either link a suspect to the scene or exclude them from the investigation. While it's not as definitive as DNA fingerprinting, it serves as a rapid and valuable preliminary tool for narrowing down possibilities.










