Understanding the Four Types of Immunity for Biology Students
Immunity forms the core protective shield of our body, preventing infections and diseases by identifying and neutralising harmful pathogens. In this simple yet comprehensive guide, we unravel the immunity definition biology concept, explore the types of immunity, shed light on immunity booster methods, and incorporate the immunity definition in nursing context to help you understand how our body preserves its healthy functioning.
What is Immunity?
In the realm of biology, immunity definition biology focuses on the body’s capacity to defend itself against invading organisms such as bacteria, viruses, fungi, parasites, and other disease-causing agents. It is a complex network of cells, tissues, and organs working in synchrony to detect and eliminate threats. From a healthcare perspective, especially in immunity definition in nursing, immunity is the body’s proactive and reactive response to foreign invaders, aiming to maintain health and well-being.
Immune System
4 Types of Immunity
When discussing the 4 types of immunity, we broadly classify them into:
Innate Immunity (also called Natural or Non-specific Immunity)
Acquired Immunity (also called Adaptive Immunity)
Active Immunity
Passive Immunity
While innate and acquired are the two main categories, active and passive immunity also play crucial roles. Let us discuss these types of immunity in more detail below.
Innate Immunity
Innate immunity is present from birth and acts as the first line of defence. It responds instantly to any pathogen attempting to invade the body. This defence system includes various barriers and cells that work collectively to prevent, detect, and destroy foreign agents before they can cause harm.
Key Barriers in Innate Immunity
Physical Barriers
Skin: Acts as a tough outer shield preventing pathogens from entering.
Body Hair and Cilia: Trap dust particles and microbes.
Mucus in the respiratory and digestive tracts traps microbes before they can invade deeper tissues.
Physiological Barriers
Stomach Acid (Hydrochloric Acid): Creates a highly acidic environment that kills pathogens in food or water.
Saliva and Tears: Contain enzymes with antibiotic properties, limiting pathogen growth.
Cellular Barriers
White Blood Cells (WBCs) such as neutrophils, lymphocytes, basophils, eosinophils, monocytes, and macrophages. These cells constantly patrol the bloodstream and tissues, ready to engulf (phagocytose) and destroy invading pathogens.
Natural Killer (NK) Cells: Recognise and eliminate virus-infected cells or tumour cells.
Cytokine Barriers
Interferons: When a virus infects a cell, the cell releases interferons that protect neighbouring cells from viral replication.
Main Cells Involved in Innate Immunity
Phagocytes: Engulf and digest foreign particles.
Macrophages: Release signalling molecules (cytokines) to recruit more immune cells.
Mast Cells: Involved in wound healing; release histamine for inflammatory responses.
Neutrophils: Release toxic granules to destroy bacteria and fungi.
Eosinophils: Contain potent enzymes targeting parasites.
Basophils: Release histamine and attack larger parasites.
Dendritic Cells: Present antigens and activate other immune cells.
Acquired Immunity
Acquired immunity, also referred to as adaptive immunity, is not present at birth. It is developed over time, often after exposure to specific pathogens or through vaccination. When the immune system first encounters a pathogen, it mounts a primary response. If the pathogen appears again, it triggers a swifter, more robust secondary response due to immunological memory.
Characteristics of Acquired Immunity
Specificity: The immune system tailors its response to particular pathogens, recognising unique antigens and neutralising them.
Diversity: It can identify a vast range of pathogens, from bacteria to parasites.
Self vs Non-Self Recognition: Normally, immune cells distinguish between the body’s own cells (self) and foreign cells (non-self).
Memory:Once exposed to a pathogen, the immune system “remembers” it. Future encounters lead to a faster, more efficient response.
Cells Involved in Acquired Immunity
B-Cells
Produced in the bone marrow.
When B-cells encounter an antigen, they differentiate into plasma cells that secrete antibodies.
Antibody-driven immune response is called humoral immunity.
T-Cells
Originate in the bone marrow and mature in the thymus.
Types include Helper T-cells (release cytokines to activate other cells), Cytotoxic T-cells (kill infected or cancerous cells), and Regulatory T-cells (regulate and moderate immune responses).
Active and Passive Immunity
Active Immunity
Develops when you come into direct contact with a pathogen or receive a vaccine containing antigens.
The body produces its own antibodies.
Usually provides long-term protection since memory cells are generated.
Passive Immunity
Occurs when ready-made antibodies are transferred from another source. Examples include maternal antibodies passed to a baby through breast milk or preformed antibodies given as medical treatment.
Offers immediate but short-lived protection (since no memory cells are formed).
Also, read the Differences between Active and Passive Immunity
Autoimmunity
Autoimmunity arises when the immune system mistakenly recognises the body’s own cells as foreign and mounts an attack against them. This leads to autoimmune disorders, such as Type I diabetes or rheumatoid arthritis. Research into immunosuppressants and targeted therapies aim to reduce the autoimmune response without compromising overall immunity.
Immunity Booster Approaches
While the body’s defence systems are highly efficient, there are practical immunity booster strategies to support your innate and acquired responses:
Balanced Diet: A nutrient-rich diet (including vitamins C, D, and E, and minerals like zinc) supports the production and functioning of immune cells.
Regular Exercise: Moderate exercise enhances circulation, helps flush out toxins, and improves immune surveillance.
Adequate Sleep: Restful sleep is crucial for repair and regeneration, allowing the immune system to stay in top form.
Stress Management: Chronic stress can suppress immune function, so adopting relaxation techniques can help balance your immune responses.
Vaccinations: Vaccines prime your immune system to recognise and respond to specific pathogens without the risk of getting a full-blown disease.
Vaccines
Vaccines form a cornerstone of acquired immunity. They contain weakened or inactive forms of pathogens or purified antigens. Once vaccinated, your immune cells produce antibodies specific to those pathogens. As a result, subsequent exposures to the actual pathogen are swiftly neutralised. Vaccination contributes to herd immunity and has successfully eradicated or reduced many infectious diseases globally.
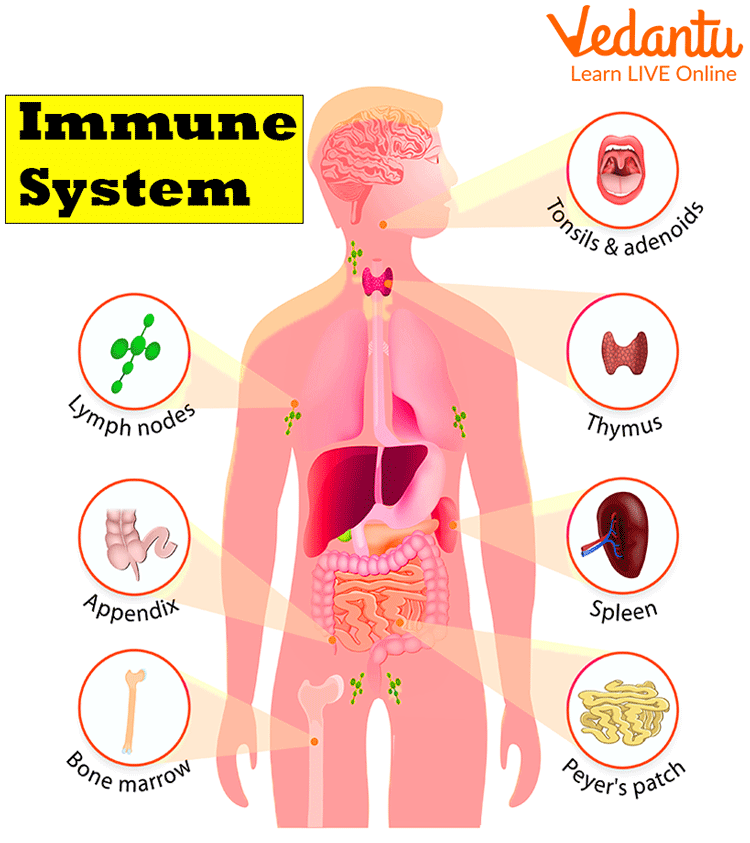
The Immune System: Organs and Components
The immune system is a large network composed of organs known as lymphoid organs, specialised cells, and molecules like antibodies. These organs produce, mature, and store immune cells, mainly lymphocytes.
Lymphoid Organs
Bone Marrow (Primary Lymphoid Organ): Production site for all blood cells, including B-cells and immature T-cells.
Thymus (Primary Lymphoid Organ): A small organ where T-cells mature.
Spleen (Secondary Lymphoid Organ): Filters the blood and destroys old or damaged blood cells. Also a site for immune cell activation.
Lymph Nodes (Secondary Lymphoid Organs): Small, bean-shaped structures along lymphatic vessels. Trap pathogens and activate lymphocytes.
Tonsils and Appendix (Secondary Lymphoid Organs): Play supportive roles in sampling pathogens entering through the mouth or digestive system.
Tertiary Lymphoid Organs: Contain fewer lymphocytes but can expand in response to inflammation or chronic infection.
Humoral vs Cell-Mediated Immune Response
Humoral Immune Response
Mediated by antibodies produced by B-lymphocytes.
When B-cells bind to an antigen, they become plasma cells that secrete specific antibodies. These antibodies can travel throughout the bloodstream to neutralise the pathogen.
Cell-Mediated Immune Response
Involves T-cells (Helper T-cells and Cytotoxic T-cells).
Helper T-cells release cytokines to coordinate the immune response.
Cytotoxic T-cells directly kill infected or abnormal cells.
The Role of Microbiome and Immunotherapy
Gut Microbiome: Recent studies highlight how beneficial gut bacteria can shape and train our immune system. A balanced gut flora can strengthen both innate and acquired immunity.
Immunotherapy: Used in cancer treatment, immunotherapy leverages the body’s own immune cells or synthetic versions to target cancer cells specifically. This cutting-edge approach includes CAR T-cell therapy and checkpoint inhibitors, illustrating how flexible and powerful our immune system can be.
Interactive Quiz on Immunity
Which of the following is NOT a physical barrier in innate immunity?
A. Skin
B. Tears
C. Body Hair
D. Mucus
Which cell type is primarily responsible for antibody production?
A. T-cells
B. B-cells
C. Dendritic cells
D. Red blood cells
Name one example of passive immunity.
A. Breastfeeding
B. Vaccination
C. Bone marrow producing antibodies
D. Mucus secretions
In autoimmunity, the immune system attacks ____:
A. Only foreign pathogens
B. The body’s own tissues
C. Only cancer cells
D. None of the above
Where do T-cells mature?
A. Bone marrow
B. Thymus
C. Spleen
D. Lymph nodes
Check your answers
B. Tears (they are a physiological barrier, not a physical one)
B. B-cells
A. Breastfeeding
B. The body’s own tissues
B. Thymus


FAQs on Immunity: How Your Body Protects Against Disease
1. What is the immune system?
The immune system is the body's defence network against harmful germs like bacteria and viruses. It's a complex system of cells, tissues, and organs that work together to keep us healthy by identifying and destroying these invaders.
2. What are the main types of immunity?
There are two primary types of immunity:
- Innate immunity: This is the general, non-specific defence system we are born with. It acts as the first line of defence against all pathogens.
- Acquired (or Adaptive) immunity: This is a more specialised defence that our body develops over time after being exposed to specific pathogens or through vaccination. It has a 'memory' to fight the same germ faster in the future.
3. What is the main difference between active and passive immunity?
The key difference is how the body gets the antibodies. In active immunity, your own body produces antibodies after an infection or vaccination, providing long-lasting protection. In passive immunity, you receive ready-made antibodies from another source (like from mother to baby), which gives immediate but temporary protection.
4. Why is innate immunity considered 'non-specific'?
Innate immunity is called non-specific because it doesn't target one particular germ. Instead, it provides a broad, general defence against any foreign substance it encounters. Think of it like a security guard that stops anyone without a pass, rather than looking for a specific person.
5. How do vaccines help our immune system protect us from diseases?
Vaccines work by introducing a harmless piece of a germ (or a weakened/dead germ) to your body. This triggers your acquired immune system to produce antibodies and memory cells without you having to get sick. If you are ever exposed to the real germ later, your immune system remembers it and can fight it off quickly and effectively.
6. How does the immune system actually fight off a virus?
When a virus enters your body, your immune system launches a multi-level attack. Innate immunity provides an initial response. Then, the acquired immune system kicks in. Special cells called T-cells identify and destroy infected body cells, while B-cells produce antibodies that neutralise the virus, preventing it from infecting more cells.
7. What happens when the immune system makes a mistake and attacks the body?
When the immune system mistakenly attacks the body's own healthy cells and tissues, it is called an autoimmune disorder. Instead of fighting foreign invaders, it identifies parts of the body as threats. Examples include Type 1 diabetes and rheumatoid arthritis.
8. What are some simple ways to support a healthy immune system?
You can support your body's defence network through healthy habits. These include eating a balanced diet rich in vitamins and minerals, getting enough sleep, exercising regularly, managing stress, and maintaining good hygiene like washing your hands.










