How to Recognize and Prevent Protein-Energy Malnutrition in Children
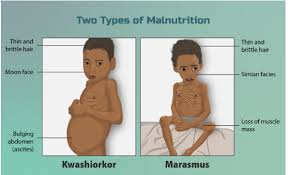
Nutritional deficiencies are a serious global concern, especially among children. Two major forms of severe malnutrition are kwashiorkor and marasmus. Both conditions arise from inadequate nutrient intake but differ in their specific causes, symptoms, and effects on the body. In this article, we will explore the difference between kwashiorkor and marasmus table, discuss kwashiorkor and marasmus symptoms, and understand their causes, treatments, and preventive measures.
What are Kwashiorkor and Marasmus?
Kwashiorkor is a form of malnutrition that primarily occurs due to severe protein deficiency. Children with kwashiorkor may receive enough calories from other nutrients, but the protein intake remains insufficient.
Marasmus, on the other hand, arises from a deficiency of both calories and proteins, along with other essential nutrients such as carbohydrates and fats. This condition is often linked to extreme poverty and chronic food scarcity.
Causes of Kwashiorkor and Marasmus
Kwashiorkor
Severe lack of protein in the diet.
A diet high in carbohydrates but low in protein.
Poor socio-economic conditions and limited access to protein-rich foods.
Marasmus
Deficiency of proteins, calories, and other nutrients (carbohydrates and fats).
Chronic starvation due to poverty, famine, or severe neglect.
Frequent infections that increase the body’s energy requirements.
Difference Between Kwashiorkor and Marasmus Table
Below is the difference between kwashiorkor and marasmus table, highlighting their key distinctions:
Kwashiorkor and Marasmus Symptoms
It is essential to recognise kwashiorkor and marasmus symptoms early to prevent long-term health complications.
Symptoms of Kwashiorkor
Oedema (swelling in the face, feet, ankles, and belly)
Thinning of muscles and limbs
Flaky or patchy skin
A fatty, enlarged liver
Changes in hair colour and texture (hair may become brittle or reddish)
Irritability and lethargy
Symptoms of Marasmus
Extreme weight loss and a very thin, emaciated appearance
Absence of subcutaneous fat
Dry, wrinkled, and loose skin
Stunted growth or reduced height for age
Muscle wasting, leaving children frail and weak
Poor appetite and frequent infections
Treatments for Kwashiorkor and Marasmus
Dietary Management
Kwashiorkor: Emphasise protein-rich foods such as pulses, dairy products, eggs, and lean meats. Gradually introduce balanced meals that include all essential nutrients.
Marasmus: Restore overall calorie intake by including carbohydrates, fats, and proteins in well-planned, frequent meals. Start slowly to avoid metabolic complications.
Medical Supervision
Both conditions may require treatment under close medical supervision.
In severe cases, hospitalisation is needed for intravenous fluids, electrolyte balance, and treatment of underlying infections.
Nutritional Supplements
Ready-to-Use Therapeutic Foods (RUTF) can help manage acute malnutrition.
Micronutrient supplements (vitamins and minerals) support faster recovery.
Prevention
Educate caregivers about balanced diets and the importance of including protein, carbohydrates, and healthy fats in meals.
Encourage breastfeeding and timely introduction of complementary foods.
Implement community programmes to improve food availability and security.
Additional Tips and Unique Insights
Include variety in meals: Consuming diverse food groups ensures a steady supply of macronutrients and micronutrients.
Monitor child growth: Regular check-ups to track height and weight can catch early signs of malnutrition.
Hygiene and sanitation: Good hygiene practices help prevent infections that can worsen malnutrition.
Community support: Charitable organisations and local food banks can aid families in poverty-stricken areas.
Quick Quiz
Which nutrient is mainly deficient in kwashiorkor?
Answer: Protein.
Name a common feature of marasmus.
Answer: Extreme weight loss or muscle wasting.
What causes fatty liver in kwashiorkor?
Answer: The lack of protein impairs the normal transport of fat, leading to its accumulation in the liver.
State one way to prevent marasmus.
Answer: Providing balanced meals that include sufficient carbohydrates, proteins, and fats.
Related Topics:


FAQs on Difference Between Kwashiorkor and Marasmus Explained
1. What is the fundamental difference between Kwashiorkor and Marasmus?
The fundamental difference lies in the primary nutritional deficiency. Kwashiorkor is caused predominantly by a severe deficiency of protein, even if calorie intake is adequate. In contrast, Marasmus results from a severe deficiency of all major nutrients—proteins, fats, and carbohydrates—leading to overall energy starvation.
2. What are the key clinical symptoms that distinguish Kwashiorkor from Marasmus?
While both are forms of malnutrition, their symptoms are distinct. Key differences include:
- Oedema: Swelling, especially in the legs, feet, and belly, is a classic sign of Kwashiorkor. This is absent in Marasmus.
- Body Appearance: A child with Kwashiorkor may not look extremely thin due to oedema, but a child with Marasmus appears severely emaciated ('skin and bones') with prominent ribs due to muscle and fat wasting.
- Skin and Hair: Kwashiorkor often causes skin lesions and changes in hair colour and texture, which is less common in Marasmus.
- Subcutaneous Fat: Some fat is preserved under the skin in Kwashiorkor, whereas it is almost completely lost in Marasmus.
3. Why do children with Kwashiorkor develop a swollen belly (oedema), while those with Marasmus appear emaciated?
This key difference is due to how the body responds to the specific nutrient lack. In Kwashiorkor, the severe protein deficiency leads to low levels of albumin in the blood. Albumin helps maintain osmotic pressure, keeping fluid within blood vessels. Without enough albumin, fluid leaks into surrounding tissues, causing oedema (swelling). In Marasmus, the body adapts to total starvation by breaking down all its reserves, including muscle and fat, for energy. This leads to severe wasting and an emaciated appearance without fluid retention.
4. What specific dietary deficiencies cause Kwashiorkor versus Marasmus?
The cause is directly linked to the diet. Kwashiorkor typically develops when a child is weaned from protein-rich breast milk onto a diet high in carbohydrates but low in protein, such as starchy gruels or cereals. Marasmus is caused by an overall lack of food, meaning the diet is deficient in calories from all sources: proteins, fats, and carbohydrates. This often occurs in infants if breastfeeding is stopped early without adequate replacement feeding.
5. Are Kwashiorkor and Marasmus common in different age groups?
Yes, there is a general pattern. Marasmus is more commonly seen in infants under one year of age due to insufficient breastfeeding or early cessation. Kwashiorkor is more typical in slightly older children, usually between 1 and 3 years, often occurring after they are weaned from breast milk to a diet lacking sufficient protein.
6. How does the treatment approach differ for a patient with Kwashiorkor compared to one with Marasmus?
While both require nutritional rehabilitation, the approach is cautious and differs initially. For Kwashiorkor, protein must be reintroduced slowly and carefully because the body's metabolism is fragile, and a sudden protein overload can be dangerous. The initial focus is on restoring electrolyte balance and providing carbohydrates and fats. For Marasmus, the primary goal is to gradually increase the overall intake of calories and all nutrients to rebuild muscle and fat stores safely.
7. What is the importance of breastfeeding in preventing conditions like Kwashiorkor and Marasmus?
Breastfeeding is crucial for preventing both forms of protein-energy malnutrition (PEM). Breast milk provides a perfect balance of proteins, fats, carbohydrates, and micronutrients required for an infant's growth. It also contains antibodies that protect the child from infections, which can worsen malnutrition. Exclusive breastfeeding for the first six months provides a complete and safe source of nutrition, significantly reducing the risk of both Marasmus and Kwashiorkor.
8. Can protein-energy malnutrition, such as Kwashiorkor, also affect adults?
Yes, although it is most common in children, protein-energy malnutrition can occur in adults. In adults, Kwashiorkor or Marasmus-like conditions can be associated with chronic illnesses like cancer or AIDS, severe gastrointestinal diseases that impair nutrient absorption, alcoholism, or extremely restrictive diets. The underlying cause is still a severe lack of protein or overall calories.