Gram-Positive vs Gram-Negative Bacteria: Cell Wall, Staining, and Exam Questions
Gram-positive and Gram-negative bacteria are the two main categories of bacteria. Scientists use a laboratory process called Gram staining to differentiate between these two groups. This distinction is based on the structure of their cell walls and their reaction to certain stains. Understanding this difference is crucial, as it affects how infections are identified and treated.
Difference Between Gram-Positive and Gram-Negative Bacteria
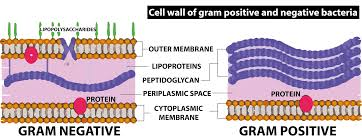
The main difference between Gram-positive and Gram-negative bacteria lies in the thickness of their cell walls and the presence of certain cell wall structures. Gram-positive bacteria possess a thick peptidoglycan cell wall, causing them to retain a blue or purple color after Gram staining. In contrast, Gram-negative bacteria have a thinner peptidoglycan wall and an additional outer membrane, resulting in a red or pink color after staining.
| Feature | Gram-Positive Bacteria | Gram-Negative Bacteria |
|---|---|---|
| Color after Gram staining | Blue or purple | Pink or red |
| Cell wall thickness | Thick peptidoglycan | Thin peptidoglycan, with outer membrane |
| Outer membrane | Absent | Present |
| Toxin type | Emetic, neurotoxin, enterotoxins | Endotoxins |
| Shapes | Spherical (cocci), rod (bacilli), or branching filaments | Sphere (cocci), rod (bacilli), spiral-shaped |
| Antibiotic resistance | Usually less resistant | Often more resistant |
| Common types |
Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus saprophyticus, Streptococcus pneumoniae, Streptococcus pyogenes, Enterococci, Corynebacterium diphtheriae, Bacillus anthracis |
Vibrio cholerae, Escherichia coli, Bartonella henselae, Campylobacter, Legionella, Salmonella, Salmonella typhi |
Understanding Gram Staining
Gram staining is a four-step process developed by Hans Christian Gram. It is used to classify bacteria and involves:
- Application of violet or methylene blue dye to bacterial cells.
- Cells are fixed and further stained, allowing the dye to enter their walls.
- Washing with a decolorizer (often alcohol).
- Application of a counterstain (typically red or pink).
Gram-positive bacteria retain the original dye and appear violet or blue. Gram-negative bacteria lose the dye during washing, then take up the counterstain and appear pink or red.
Characteristics and Health Significance
Gram-positive bacteria lack an outer membrane and are more likely to respond to antibiotics like penicillin. They may produce toxins such as emetic toxin or neurotoxins, leading to foodborne illnesses, skin infections, and other diseases.
Gram-negative bacteria possess an outer membrane that provides additional protection and resistance. Disruption of their wall can release endotoxins, sometimes causing severe reactions in the host. They are a leading concern in public health due to antibiotic resistance and their ability to cause outbreaks of diseases such as cholera and typhoid fever.
Examples of Gram-Positive Bacteria and Related Diseases
- Staphylococcus aureus – can cause skin infections and, in severe cases, blood infections.
- Staphylococcus epidermidis – major cause of catheter or device-related infections.
- Streptococcus pneumoniae – causes pneumonia and meningitis.
- Streptococcus pyogenes – responsible for throat infections, skin infections, and sometimes rheumatic fever.
- Enterococci – present in the intestines, but can lead to urinary tract or bile duct infections.
- Corynebacterium diphtheriae – causes diphtheria, affecting the throat and sometimes the skin.
- Bacillus anthracis – leads to anthrax, an infectious disease affecting both animals and humans.
Examples of Gram-Negative Bacteria and Related Diseases
- Vibrio cholerae – causes cholera, a serious diarrheal illness.
- Escherichia coli – can lead to diarrhea, urinary tract infections, or food poisoning.
- Bartonella henselae – causes cat scratch disease, transmitted by infected cats.
- Campylobacter – a major cause of bacterial diarrhea. Often contracted from undercooked poultry.
- Legionella – responsible for Legionnaires’ disease, a severe form of pneumonia acquired by inhaling contaminated water droplets.
- Salmonella (including Salmonella typhi) – causes food poisoning and typhoid fever.
Treatment and Antibiotic Resistance
Most Gram-positive infections are responsive to a broad range of antibiotics, including penicillin and tetracyclines. Gram-negative infections, because of the protective outer membrane, are often more challenging to treat. These bacteria may require more specific antibiotics, such as ciprofloxacin or azithromycin, and are known to become resistant to drugs more rapidly.
Preventing Antibiotic Resistance
Limiting antibiotic resistance starts with using antibiotics only when prescribed. People can help prevent resistance and the spread of infection by following hygiene practices, such as regular handwashing, food safety, keeping vaccinations up to date, and avoiding the use of leftover or unapproved antibiotics.
Summary Table
| Aspect | Gram-Positive | Gram-Negative |
|---|---|---|
| Stain color | Blue/purple | Red/pink |
| Wall structure | Thick peptidoglycan, no outer membrane | Thin peptidoglycan, with outer membrane |
| Resistance to antibiotics | Generally lower | Generally higher |
| Toxins | Produces exotoxins | Releases endotoxins |
Explore Related Biology Topics
Practice Question
Identify one key structural feature that makes Gram-negative bacteria more resistant to antibiotics than Gram-positive bacteria.
For more detailed explanations, examples, and interactive resources, explore biology lessons and practice exercises at Vedantu.


FAQs on Difference Between Gram-Positive and Gram-Negative Bacteria
1. What is the difference between Gram-positive and Gram-negative bacteria?
Gram-positive bacteria have a thick peptidoglycan cell wall that retains the crystal violet stain, appearing purple under a microscope. Gram-negative bacteria have a thin peptidoglycan layer and an outer membrane containing lipopolysaccharides; they do not retain the crystal violet stain and instead appear pink/red after counterstaining. Key differences include:
- Cell wall thickness (thicker in Gram-positive)
- Presence of outer membrane (only in Gram-negative)
- Stain retention during Gram staining
- Antibiotic resistance (higher in Gram-negative)
2. Why do Gram-positive bacteria retain the crystal violet stain?
Gram-positive bacteria retain the crystal violet stain because their thick peptidoglycan layer traps the dye-mordant complex during the decolorization step. As a result, they appear purple under a microscope after the Gram staining process.
3. Which type of bacteria is more resistant to antibiotics: Gram-positive or Gram-negative?
Gram-negative bacteria are generally more resistant to antibiotics. Their outer membrane acts as a barrier, limiting the entry of many antibiotics and making treatment more challenging.
4. What is the function of the outer membrane in Gram-negative bacteria?
The outer membrane in Gram-negative bacteria:
- Provides protection against hostile environments and antibiotics
- Contains lipopolysaccharides, which can trigger immune responses
- Acts as a barrier to certain chemicals and dyes
5. List two examples each of Gram-positive and Gram-negative bacteria and their associated diseases.
Gram-positive examples:
- Streptococcus pneumoniae - causes pneumonia
- Staphylococcus aureus - causes skin infections
Gram-negative examples:
- Escherichia coli - causes urinary tract infections
- Neisseria meningitidis - causes meningitis
6. Describe the steps of the Gram staining procedure.
The Gram staining process involves:
- Application of crystal violet dye
- Addition of iodine (mordant)
- Alcohol wash for decolorization
- Counterstaining with safranin
This sequence differentiates between Gram-positive and Gram-negative bacteria by color under a microscope.
7. Why are Gram-negative bacterial infections often more difficult to treat?
Gram-negative bacterial infections are harder to treat because the outer membrane blocks many antibiotics and contains enzymes that degrade them, leading to higher levels of antibiotic resistance.
8. What key components are found only in the cell wall of Gram-positive bacteria?
Gram-positive bacterial cell walls uniquely contain teichoic acids and have a much higher percentage of peptidoglycan compared to Gram-negative bacteria.
9. How does the structure of Gram-negative bacteria contribute to their pathogenicity?
Gram-negative bacteria have an outer membrane with lipopolysaccharides (LPS), which:
- Helps evade the host immune system
- Releases endotoxins when bacteria die, worsening infections
- Provides increased resistance to environmental threats and antibiotics
10. Explain the clinical importance of distinguishing between Gram-positive and Gram-negative bacteria.
Distinguishing Gram-positive from Gram-negative bacteria is crucial because treatment strategies and antibiotic choices differ for each type. Correct identification guides effective therapy and improves patient outcomes.
11. What roles do teichoic acids play in Gram-positive bacteria?
Teichoic acids in Gram-positive bacteria:
- Stabilize the cell wall structure
- Help bind positively charged ions
- Play a role in cell growth and division
12. How can students remember the core differences between Gram-positive and Gram-negative bacteria for exams?
Tips to remember:
- Gram-Positive = Purple stain & Peptidoglycan is thick
- Gram-Negative = Not purple (pink/red) & has extra outer membrane
- Recall common examples using mnemonics (e.g., "Staph & Strep are strong Gram-positive friends")










