How Blood Components Work Together in the Human Body
Blood is more than just a red fluid coursing through our veins. It is a fluid connective tissue with varied roles, from carrying oxygen and nutrients to defending our body against infections. In this detailed guide, you will learn what is blood, its structure, the composition of blood, blood cell types, and the function of blood in the human body. We will also discuss the formation of blood and highlight some unique facts not commonly covered elsewhere. By the end of this page, you will have a thorough understanding of why blood is vital to life.
Read More: Tissues
Introduction:
Blood circulates through our body, delivering oxygen and vital nutrients to cells and carrying away carbon dioxide and other wastes. It makes up about 7-8% of the total body weight in a healthy adult, and an average adult typically has around 5-6 litres of blood.
Despite appearing as a single uniform fluid, blood is made of multiple components, each with its special role. We often depict blood as “red,” but its colour and characteristics depend on a unique protein called haemoglobin, as well as other dissolved components.
Structure of Blood
When discussing the structure of blood, we mean the physical and organisational aspects of its components. Blood moves within a closed circulatory system comprising the heart and an extensive network of blood vessels (arteries, veins, and capillaries). Within this system:
Red Blood Cells (RBCs), packed with haemoglobin, transport oxygen to tissues.
White Blood Cells (WBCs) defend against infection.
Platelets, also called thrombocytes, help in clot formation.
The liquid medium, plasma, carries nutrients, hormones, and other essential substances.
Composition of Blood
One of the most critical aspects of understanding blood is grasping the composition of blood. Essentially, blood consists of two main parts:
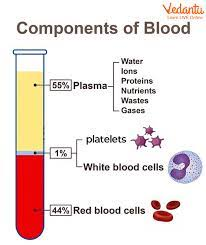
A blood diagram often shows the relative proportions of these components, highlighting that blood is about 55% plasma and 45% formed elements of blood (RBCs, WBCs, and platelets).
Plasma (about 55%)
Water: Forms the bulk of plasma (around 90-92%).
Proteins: Such as fibrinogen, albumin, and globulins.
Solutes: Including electrolytes (salts), nutrients (glucose, amino acids), gases, hormones, and waste products.
Formed Elements of Blood (about 45%)
Red Blood Cells (RBCs) or Erythrocytes: These biconcave, disc-shaped cells contain haemoglobin.
White Blood Cells (WBCs) or Leucocytes: The “soldiers” of the immune system.
Platelets (Thrombocytes): Tiny fragments essential for blood clotting.
By separating a sample of blood in a centrifuge, these components are segregated into distinct layers: plasma (top), a thin buffy coat (WBCs and platelets), and RBCs (bottom). Recognising the composition of blood clarifies how blood is both a transport system and an active participant in immunity.
Read More: Difference Between Plasma and Serum
Blood Cells Types
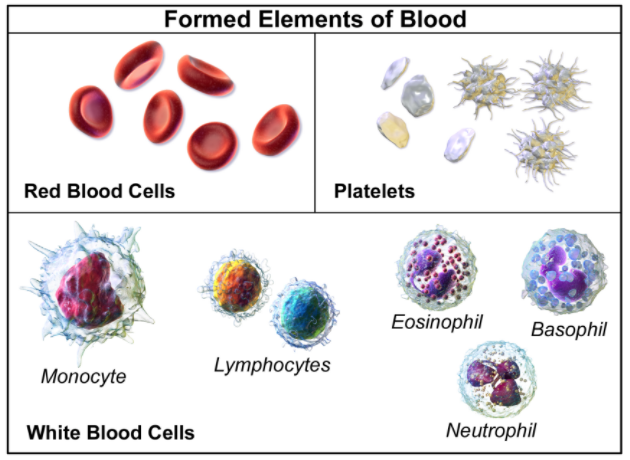
A deeper look into the blood cell types reveals their specialised roles. Blood consists of three main types of cells:
1. Red Blood Cells (Erythrocytes)
Shape and Structure: RBCs are biconcave discs without a nucleus in humans.
Function: Primary carriers of oxygen (via haemoglobin) and carbon dioxide.
Lifespan: Approximately 120 days, after which they are broken down primarily in the spleen.
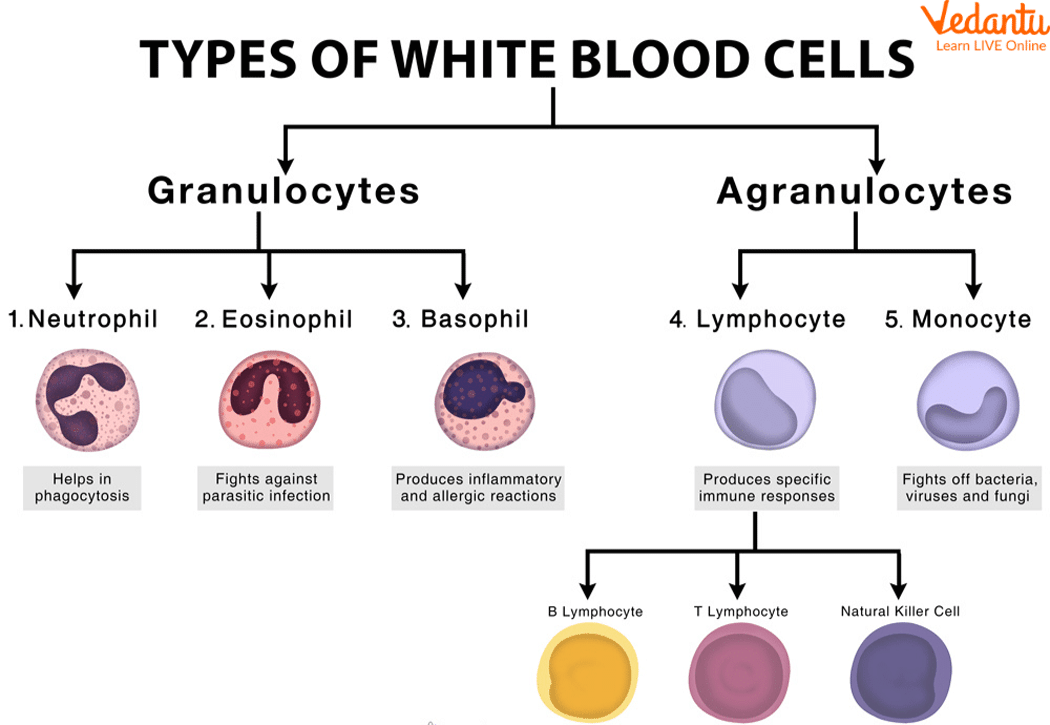
2. White Blood Cells (Leucocytes)
Function: Major players in immune defence, fighting infections from bacteria, viruses, and other pathogens.
Types of WBCs:
Granulocytes (with visible granules in the cytoplasm):
Neutrophils: The most abundant WBCs, crucial for phagocytosing bacteria.
Eosinophils: Combat parasitic infections and help regulate allergic responses.
Basophils: Release histamine and heparin, significant in inflammation and allergic reactions.
Agranulocytes (lack visible granules in the cytoplasm):
Monocytes: Mature into macrophages in tissues and clean up cellular debris.
Lymphocytes: Include B-lymphocytes and T-lymphocytes, vital for adaptive immunity and antibody production.
3. Platelets (Thrombocytes)
Appearance: Tiny, disc-like fragments derived from megakaryocytes in the bone marrow.
Main Function: Assist in clotting and coagulation, forming plugs at wound sites to prevent blood loss.
Formation of Blood (Haematopoiesis)
The formation of blood, scientifically called haematopoiesis, occurs primarily in the red bone marrow (found in bones such as the sternum, ribs, and pelvis). Stem cells in the bone marrow differentiate into various blood cell types—RBCs, WBCs, and platelets—under the influence of specific growth factors.
Key Steps in Haematopoiesis
Pluripotent Stem Cells: The origin of all blood cells.
Commitment to Lineages: Some become myeloid stem cells (leading to RBCs, platelets, granulocytes, and monocytes), while others become lymphoid stem cells (leading to lymphocytes).
Maturation: Cells develop the unique characteristics needed for their final function (e.g., RBCs fill with haemoglobin, and lose their nucleus).
Release into Circulation: Mature cells enter the bloodstream, ready to perform the function of blood in the human body.
Understanding the formation of blood is crucial for comprehending various disorders like anaemia (reduced RBC production), leukopenia (low WBC count), and thrombocytopenia (low platelet count).
Also Check: Difference Between Blood and Lymph
The Function of Blood in the Human Body
What exactly is the function of blood in the human body? Broadly, it can be divided into the following key roles:
Transportation
Oxygen and Carbon Dioxide: RBCs carry oxygen from the lungs to tissues and bring back carbon dioxide to the lungs for exhalation.
Nutrients and Waste: Blood carries glucose, amino acids, vitamins, and minerals to cells while removing metabolic wastes like urea.
Hormones: Endocrine glands release hormones directly into the bloodstream for delivery to target organs.
Regulation
Temperature: Blood helps distribute heat throughout the body and assists in thermoregulation.
pH and Fluid Balance: Plasma contains buffers to maintain pH balance; it also regulates fluid and electrolyte balance.
Protection
Immune Defence: WBCs identify and destroy pathogens.
Blood Clotting: Platelets and clotting factors prevent excessive blood loss from injuries.
By fulfilling these functions, blood ensures the survival and efficient operation of every tissue and organ. Though these are often summarised as the main function of blood, the detail above shows how multifaceted these roles can be.
Blood Vessels
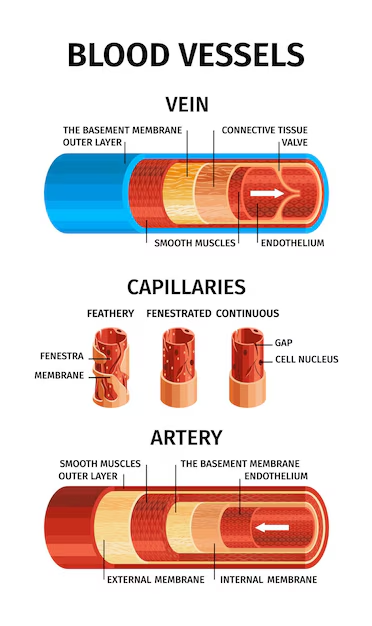
Blood doesn’t simply exist in isolation; it is transported through an intricate network of blood vessels:
Arteries
Carry oxygen-rich blood away from the heart.
Their walls are thick and elastic to withstand high pressure.
Veins
Return deoxygenated blood to the heart.
Thinner walls often contain valves to prevent backflow.
Capillaries
Microscopic vessels where exchange of gases, nutrients, and waste occurs.
Connect the arterial and venous systems.
Additionally, sinusoids are specialised, wider capillaries in organs like the liver and spleen, allowing efficient exchange of larger molecules or even cells.
Additional Unique Facts about Blood
Here are a few unique tidbits to make our content stand out from the rest:
Role of Erythropoietin (EPO): A hormone primarily produced by the kidneys that stimulates the formation of blood cells, especially RBCs. It responds to low oxygen levels, signalling the bone marrow to produce more RBCs.
Unique Vertebrate without Haemoglobin: The Antarctic icefish lacks haemoglobin, relying on the oxygen-rich cold waters for its survival—an exception among vertebrates.
Blood Groups and Transfusion: Beyond the well-known ABO system, there are dozens of lesser-known blood group systems such as Rh, Kell, and Duffy. Proper blood typing is crucial to avoid transfusion reactions.
Colour Variations in Other Organisms: While human blood is red due to haemoglobin, some organisms have different-coloured blood: for instance, many arthropods have blue blood due to a copper-based molecule called haemocyanin.
White Blood Cell Lifespan: Unlike RBCs, some WBCs (like certain memory lymphocytes) can live for years, offering long-term immunity after infections or vaccinations.
Related Links:


FAQs on Blood: Structure, Formation, Composition, and Core Functions
1. What are the main components of blood and their general percentages?
Blood is composed of two main parts: plasma, a liquid matrix that makes up about 55% of blood volume, and formed elements, which constitute the remaining 45%. The formed elements include red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes).
2. What are the vital functions of blood in the human body?
The vital functions of blood are critical for survival and can be categorised as follows:
- Transport: It carries oxygen from the lungs to tissues, and carbon dioxide from tissues back to the lungs. It also transports nutrients, hormones, and waste products.
- Regulation: Blood helps maintain body temperature, pH balance, and fluid volume in the circulatory system.
- Protection: It prevents blood loss through clotting and fights infections through the actions of white blood cells and antibodies.
3. Why is blood classified as a fluid connective tissue?
Blood is considered a specialised connective tissue because, like other connective tissues, it consists of cells suspended in an extracellular matrix. In the case of blood, the cells are the formed elements (RBCs, WBCs, platelets), and the fluid extracellular matrix is the blood plasma.
4. What are the different types of blood cells and their primary roles?
There are three main types of blood cells:
- Red Blood Cells (RBCs or Erythrocytes): These are responsible for oxygen transport, facilitated by the protein haemoglobin.
- White Blood Cells (WBCs or Leukocytes): They are the key players in the immune system, defending the body against pathogens. They include neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
- Platelets (Thrombocytes): These are small cell fragments that play a crucial role in blood clotting to prevent excessive bleeding.
5. What is the specific importance of haemoglobin in the function of blood?
Haemoglobin is a protein found inside red blood cells that contains iron. Its primary importance is to bind with oxygen in the lungs and transport it to all the body's tissues. It also plays a role in transporting carbon dioxide, a waste product, from the tissues back to the lungs to be exhaled.
6. How does the biconcave shape of a red blood cell enhance its function?
The biconcave disc shape of a mature red blood cell is a crucial structural adaptation. This shape increases the cell's surface-area-to-volume ratio, which facilitates more efficient diffusion of oxygen and carbon dioxide across its membrane. Additionally, it provides flexibility, allowing RBCs to squeeze through narrow capillaries that may be smaller than their own diameter.
7. What is the key difference between blood plasma and serum?
The primary difference lies in the presence of clotting factors. Plasma is the liquid component of blood that holds blood cells in suspension and contains proteins, including clotting factors like fibrinogen. Serum is the fluid that remains after the blood has been allowed to clot, meaning it is essentially plasma without the fibrinogen and other clotting factors.
8. How does the process of blood coagulation work to stop bleeding?
Blood coagulation, or clotting, is a complex cascade of events initiated in response to an injury. Platelets first aggregate at the injury site to form a temporary plug. This triggers a series of enzymatic reactions involving various clotting factors. The final step in this cascade is the conversion of the soluble protein fibrinogen into insoluble fibrin threads, which form a mesh that traps red blood cells and platelets, creating a stable clot.
9. What determines a person's blood group in the ABO system?
A person's blood group in the ABO system is determined by the presence or absence of specific antigens on the surface of their red blood cells.
- Group A has A antigens.
- Group B has B antigens.
- Group AB has both A and B antigens.
- Group O has neither A nor B antigens. This is crucial for ensuring compatibility during blood transfusions.
10. Why is an individual with the AB blood group called a 'universal recipient'?
An individual with blood group AB is called a 'universal recipient' because their red blood cells have both A and B antigens on their surface. Consequently, their blood plasma does not contain antibodies against either A or B antigens (no anti-A or anti-B antibodies). This absence of antibodies means they can receive blood from any ABO group (A, B, AB, or O) without triggering an immune reaction.
11. Why is the Rh factor a concern for an Rh-negative mother during a second pregnancy with an Rh-positive foetus?
During the birth of her first Rh-positive baby, some of the baby's blood can enter the Rh-negative mother's circulation, causing her immune system to produce anti-Rh antibodies. In a subsequent pregnancy with another Rh-positive foetus, these maternal antibodies can cross the placenta and attack the foetus's red blood cells, leading to a condition called erythroblastosis fetalis, which can cause severe anaemia and jaundice in the newborn.
12. Where are blood cells produced in the human body?
The formation of blood cells, a process known as haematopoiesis, primarily occurs in the red bone marrow. In adults, this is mainly found in the bones of the pelvis, sternum, ribs, and vertebrae. All types of blood cells—red blood cells, white blood cells, and platelets—originate from a common type of stem cell in the marrow.










